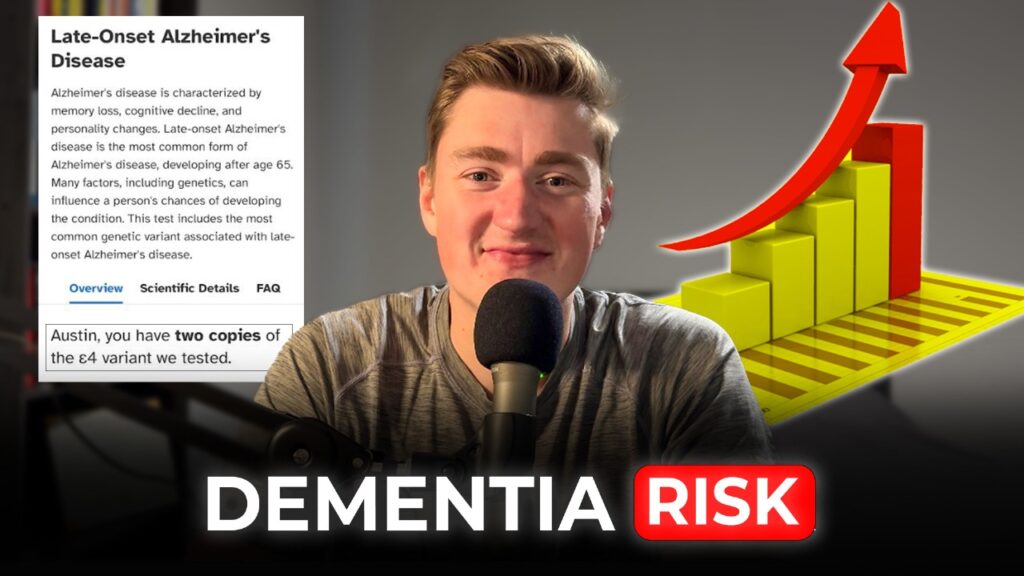
Earlier this year, I took a 23andMe genetic test and discovered I carry two gene variants associated with up to a 15-fold increased risk of Alzheimer’s. But I’m not really concerned. Let me explain why.
Contents
The APOE Gene and Alzheimer's Risk
This gene, called APOE (Apolipoprotein E), comes in three variants: APOE2, APOE3, and APOE4. We inherit one copy from each parent.
APOE Variants:
APOE ε2: Rare (5-10% of the population). Protective against Alzheimer’s.
APOE ε3: Common (60-75% of the population). Neutral, no significant effect on risk.
APOE ε4: (15-20% of the population). Increases risk
- One copy (ε3/ε4): 2-3 times higher risk.
- Two copies (ε4/ε4): 8-15 times higher.
Nevertheless, it’s crucial to understand that APOE, or APOE4, does not cause Alzheimer’s disease. Genes do not determine your longterm health and disease fate. While genetic may load the gun, it’s lifestyle, environment, and metabolic health that pull the trigger.
While my two copies of APOE4 may indicate a higher risk, I believe my approach to health and prevention will make all the difference.
Alzheimer's: A Metabolic Disease?
There’s a growing body of evidence suggesting Alzheimer’s is less a genetic inevitability and more a metabolic disease. It’s driven by factors like poor diet, sedentary behavior, chronic stress, and disrupted sleep—lifestyle choices that are increasingly common in modern society.
Alzheimer’s pathology is classically characterized by the buildup of beta-amyloid plaques, sticky clumps of protein that disrupt brain function. But what drives this plaque formation? Research points to oxidative stress, inflammation, and metabolic dysfunction (specifically, our bodies decline in ability to use glucose for energy in the brain).
Brain Glucose Hypometabolism: The Root Cause?
One key finding is that Alzheimer’s brains struggle to use glucose for energy, a condition known as cerebral glucose hypometabolism. This energy crisis is caused by insulin resistance in the brain, earning Alzheimer’s the nickname “Type 3 Diabetes.” A seriously silly name, as diabetes means “increased urine”. A better name would be insulin resistance of the brain.
Insulin is required to transport glucose into cells, and when this process falters, the brain experiences an energy deficit that impairs its ability to function optimally. This decline in energy metabolism contributes to the cognitive decline and memory loss characteristic of Alzheimer’s disease.
While glucose metabolism declines, the ability to use ketones as an alternative energy source remains intact—a critical insight with major implications for prevention (and treatment). Ketones, produced during fat metabolism or through a ketogenic diet, can bypass the insulin-dependent pathways and provide the brain with a readily available and efficient energy source. This opens the door to therapeutic strategies centered around ketogenic diets, exogenous ketones, or other interventions aimed at restoring energy balance in the brain.
Evidence Supporting the Metabolic Theory
Several studies support the idea that Alzheimer’s is more about poor metabolic health. And that environment and lifestyle play a significant role in risk:
Brain Metabolic Dysfunction at the Core of Alzheimer’s Disease
- This study explores the idea that “Alzheimer’s disease (AD) is fundamentally a metabolic disease”. It emphasizes how brain insulin and IGF resistance contribute to the structural and functional abnormalities characteristic of AD. This metabolic dysfunction may underlie the disease’s progression.
Central obesity and increased risk of dementia more than three decades later
- This study shows a strong correlation between central obesity—a marker of poor metabolic health—and an increased risk of dementia. Individuals with larger waist circumferences were found to be three times more likely to develop dementia.
- This study compared three groups: healthy controls, individuals with mild cognitive impairment, and those with AD. It found that glucose metabolism in the brain was significantly impaired in the latter two groups. However, ketone metabolism remained intact, suggesting alternative metabolic pathways could play a therapeutic role.
- This study comparing genetically identical communities in Africa and the United States found large differences in dementia rates. Those living in healthier environments in Africa exhibited dramatically lower rates of dementia, despite sharing the same genetic risks. This highlights the profound impact of lifestyle and environment on cognitive health.
Modern Disease & Poor Metabolic Health
It’s worth noting that the risk associated with APOE4 has increased in recent decades, likely due to lifestyle shifts. For example, older studies suggested APOE4 only modestly increased Alzheimer’s risk. Now, with only 7% of U.S. adults considered metabolically healthy, that risk has skyrocketed.
Importantly, dementia and Alzheimer’s disease are not inevitable consequences of aging. Instead, they are largely modern conditions linked to poor metabolic health and lifestyle factors.
Why APOE4 Increases Risk
The APOE gene produces a protein involved in lipid metabolism, including clearing beta-amyloid from the brain. The APOE4 variant is structurally less efficient and more prone to damage, which amplifies the risk of plaque buildup, inflammation and ultimately cognitive decline:
- Dysfunctional HDL
- APOE4 carriers are more prone to oxidative stress, which damages HDL particles—the “garbage trucks” responsible for clearing beta-amyloid. As damaged HDL particles become less effective, harmful plaques are left behind.
- Blood-Brain Barrier Damage
- Dysfunctional HDL activates enzymes like MMP-9, which disrupt the blood-brain barrier, allowing harmful substances to enter the brain.
- Another study found that APOE 4 carriers exhibit significantly higher BBB dysfunction caused by MMP-9 predicting cognitive decline.
- Excessive Glycation
- APOE4 binds more aggressively to sugar-damaged proteins (advanced glycation end products, or AGEs), accelerating plaque formation.
- The above study showed APOE4 is damaged by glycation at three times the rate of the APOE3 variant.
In short, carrying APOE4 creates a “perfect storm” for metabolic dysfunction in the brain:
Carry APOE4 → Damaged HDL → Impaired Plaque Clearance & BBB Disruption → Accelerated Neurodegeneration
BUT, with the right interventions I believe this storm can be avoided.
Genes Are Not Destiny
Even with APOE4, Alzheimer’s isn’t inevitable—it’s preventable. By optimizing your metabolic health and reducing oxidative stress, you can significantly lower your risk. This includes strategies like:
- Low-Carb and Ketogenic Diets: These improve insulin sensitivity provide ketones as an alternative brain fuel, and reduce both inflammation and oxidative stress.
- Exercise: Regular physical activity improves glucose metabolism, reduces inflammation and supports brain health. Exercise has been shown to be the most effective elixir for prolonging cognitive function.
- Stress Management: Chronic stress drives oxidative damage; mindfulness, good sleep hygiene, and relaxation techniques are powerful antidotes.
Remember, your genes may load the gun, but your lifestyle pulls the trigger.
Ketones: A Game-Changer for Brain Health
Ketones are emerging as a powerful tool for Alzheimer’s prevention and management. While glucose metabolism declines in Alzheimer’s patients, ketone metabolism remains functional, which can serve as a critical backup energy source.
Low Carb/Ketogenic Diets:
- A cross-sectional study found that ketones can support brain energy metabolism and improve function in Alzheimer’s patients. (Study)
- A modified ketogenic diet increased brain activity and improved cerebrospinal fluid biomarkers in at-risk individuals. (Study)
- Low-carb diets have been shown to reverse existing brain deterioration and improve network stability, a biomarker for brain aging. (Study)
Exogenous Ketones:
Supplementing with ketones has shown promise in restoring brain energy levels and improving cognitive performance in patients with AD.
- A ketone monoester supplement showed significant improvements in cognitive functions, including verbal fluency, demonstrating the potential of ketones to mitigate cognitive decline (study).
- MCT based ketogenic formula improved both cognitive and physical performance in patients with AD (study).
- MCT oil (which boosts ketone production) had positive effects on cognition in mild to moderate AD patients with APOE4 (study).
This is why I prioritize a low-carb, ketogenic lifestyle. Beyond prevention, it offers immediate benefits like improved focus, energy, and mental clarity. It’s certainly an essential component of my approach to optimal brain health.
The Bottom Line
Carrying APOE4 doesn’t mean you’re destined for Alzheimer’s. It simply means your brain and body are more sensitive to the effects of poor metabolic health. By taking charge of your diet, exercise, and overall lifestyle, you can dramatically lower your risk.
Understanding your genetic risk isn’t about fear; it’s about empowerment. If you’re curious about your genetic profile, consider getting tested and use the knowledge to take proactive steps. For me, learning about my APOE4 status has been a powerful motivator to continue optimizing my health—and it can be for you, too.
Best,
Austin
The Art of Optimal Living
Watch The YouTube Video
Learn effective strategies for optimizing your health every single week.